Diarrhoea, dysentery, and persistent diarrhoea in children: Case discussions & prescription guide by Dr. Balaji Chinnaswami
M3 India Newsdesk Sep 25, 2019
Dr. Balaji Chinnaswami provides quick evidence-based diagnosis and prescription guide for distinguishing between diarrhoea, dysentery, and persistent diarrhoea in infants and children.

Key practice points
- Most of the diarrhoeal episodes are viral in aetiology and do not require antibiotics
- Oral rehydration and zinc supplements need to be prescribed
- Antibiotics are recommended for dysentery but metronidazole combinations should be avoided as amoebiasis is rare in children
Diarrhoea
A one-year-old boy weighing 10 kg presents with loose stools for two days. He has mild fever and two episodes of vomiting; no blood in stools.
Science behind management
Diarrhoea is mostly caused by viruses or enterotoxigenic E. coli. It is self-limiting and there is no need for antibiotics.
- Oral rehydration solution and zinc supplements are the treatment options.
- A thirsty irritable child with sunken eyes is dehydrated and may need extra fluids.
- A lethargic child with poor intake and sunken eyes may need hospitalisation.
Investigations to run
Stool routine and stool culture are not indicated routinely.
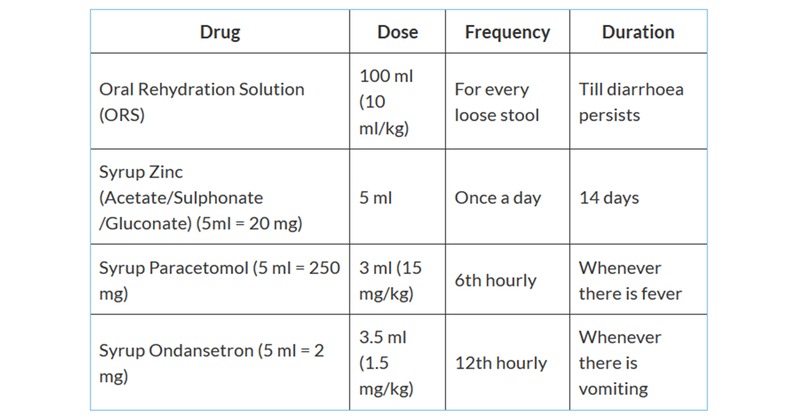
Rx
Advice to give to parents
- Continue breastfeeding and feed well-cooked, mashed cereal based diet, bananas and yoghurt.
- Give extra fluids like tender coconut water, lassi, butter milk.
- Report to casualty immediately if the child shows danger signs like convulsions, lethargy, or unconsciousness, is not able to drink or breastfeed, is vomiting everything, has not passed urine in six hours.
Dysentery
A 3-year-old girl weighing 12 kg presents with fever for two days, passing frequent but small quantities of bloody mucoid stools associated with painful defecation (tenesmus).
Science behind management
- Shigella is the commonest cause of dysentery. Amoebiasis is uncommon, so avoid Metronidazole-like combinations.
- Antibiotics are indicated in dysentery. Fluroquinolones are currently recommended as first line therapy.
- Not all bloody stools are dysentery. For a child with intermittent episodes of crying and vomiting along with bloody stools, first rule out intussusception by USG abdomen.
Investigations to run
Stool examination for amoebiasis if the child is not responding to antibiotics.
Rx

Advice to give to parents
- Ensure that the child stays adequately hydrated by giving extra fluids like tender coconut water, butter milk, lassi etc.
- Continue giving well-cooked cereal based diet, fruits and vegetables.
- Report to casualty immediately if you notice danger signs like convulsions, lethargy, or unconsciousness, if the child is not able to drink or breastfeed, is vomiting everything, has not passed urine in six hours.
- Review after 48 hours if the child doesn’t respond to treatment. Antibiotics need to be changed in such cases.
Persistent Diarrhoea
A 10-month old baby presents with fifteen days history of diarrhoea. Previously it was watery multiple times happening day & night. Now for the last four days it is not present during night. There is perianal excoriation.
Science behind management
- Infections damage intestinal mucosa and cause lactase deficiency leading to temporary lactose intolerance.
- Lactase deficiency causes osmotic diarrhoea I.e. diarrhoea only when feeds are given, hence diarrhoea less frequent during night than day time.
- Antibiotics for prolonged diarrhoea is not the solution. Cutting out lactose containing dairy products from diet and continuation of breastfeeding is all that is needed.
Investigations to run
Stool for pH <5.5 and presence of reducing substances is suggestive of lactose intolerance. Make sure analysis is done in the liquid part of stools.
Rx

Advice to give to parents
- Cut out lactose containing milk and dairy products from the diet for 8 weeks.
- Continue breastfeeding. Breastmilk doesn't worsen osmotic diarrhoea.
- Feed bread and cereals, fruits and vegetables. Meat and fish can be eaten.
To read the previous article in this series, click Is it viral or bacterial? Evidence-based disease management & case discussions by Dr. Balaji Chinnaswami
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Balaji Chinnaswami is a professor of Paediatrics at a reputed medical college in Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries