How to discuss palliative care and when to initiate it?: Dr. Rajam Iyer
M3 India Newsdesk Jul 10, 2019
Healthcare professionals around the globe are trained to save lives. The training sadly falls short in preparing doctors to deal, discuss about a certainty of life: Death and Dying. In this article, Dr. Rajam Iyer, a palliative care expert discusses why doctors should discuss hospice with patients and when they can initiate it.
Why talk about palliative care?
I was asked to review a 56-year old patient as a pulmonary palliative care physician. I noticed that he was having a respiratory rate of 28 per minute, with bouts of distressing dry cough. He has had chronic renal disease since 4 years and was presently on dialysis thrice a week. Over the course of 4 months prior to this, he had suffered 2 myocardial infarctions, with an ejection fraction at 20%. He also had a deep vein thrombus in his right calf.
How can we make him comfortable? What choices do we have? Does medicine always cure? What must a doctor do when modern medicine has nothing to offer?
Health care professionals around the globe are trained to save lives. The training sadly falls short in preparing doctors to deal, discuss about a certainty of life: Death and Dying. Doctors end up delaying death, which is often thought as saving lives. Only a few are trained in end-of-life conversations.
The Lancet 2015 quality of death index report, ranks India amongst 15 worst countries to die in. We need a better understanding of basic medical ethics, concepts of palliative care, what happens during active dying and how to keep someone comfortable at end of life, to avoid bad deaths.
One in 5 suicides in India are due to health related issues. Death is considered as a failure by doctors, like a problem to be solved not rather than a process to be lived. Many of us live in denial about death and according to ‘Dying Matters Coalition’, 8 out of 10 people are uncomfortable discussing death.
Today, approximately 8.5 to 10 million Indians die annually. Statistics show 10% die suddenly. The rest go through varying periods of being bed-bound.
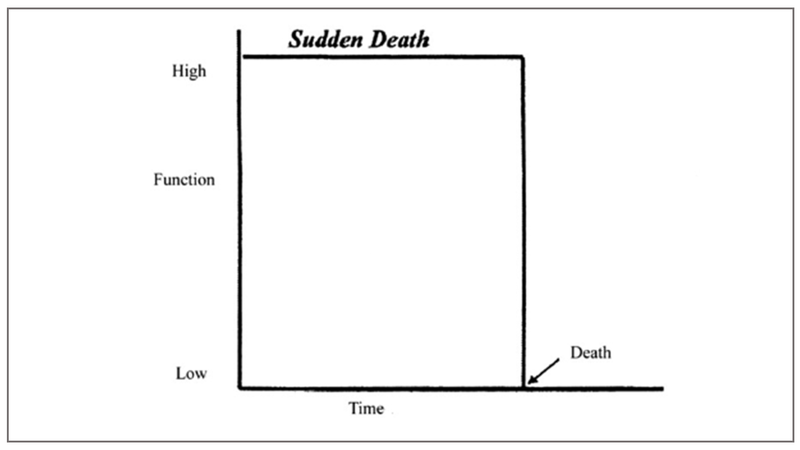
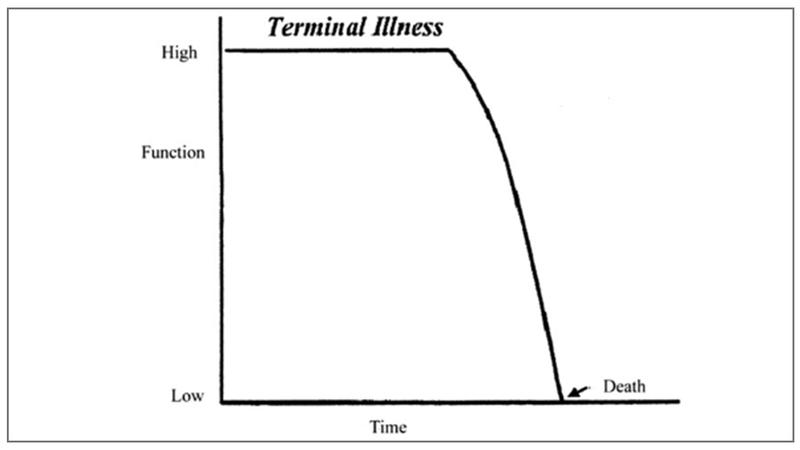
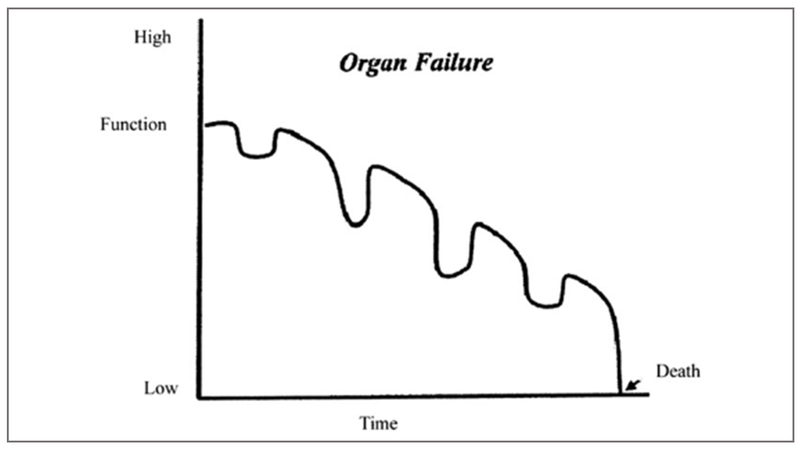
The trajectories leading to death can be broadly divided into 4 categories*
Sudden Death, where the person enjoys good quality of life and suddenly dies, for example, myocardial infarction, accidents, pulmonary embolism.
Terminal illness, such as in cancer, where a person suffers from a terminal illness, maintains a decent quality of life and then declines to death.
Chronic illnesses, such as organ failure (congestive cardiac failure), chronic obstructive pulmonary disease, interstitial lung disease, chronic renal failure, and neuro-degenerative illnesses. In these conditions patients live for prolonged periods of time with high symptom burden. Acute worsening due to infections, decompensation frequently punctuates the natural course of their illness. Each of these could lead to hospitalisation, ICU admission, or even death. However, if the patient survives the acute crisis, there is almost always a significant drop in quality of life. They do live longer but not necessarily well.
Fraility and Dementia in the elderly. Here the quality of life remains poor for a prolonged time, with increasing dependence and the patient slowly fades till death.
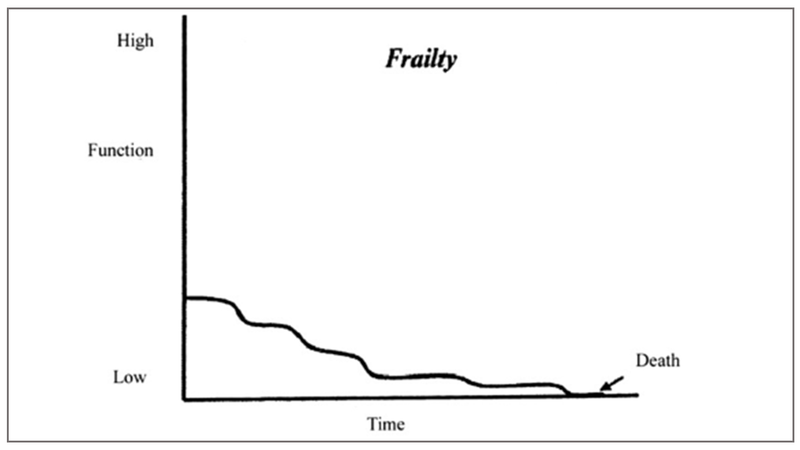
In all these trajectories, the patient and his family endure not just physical but emotional, psychological, spiritual and in a country like India, where out of pocket expenses are high, financial stress too. It is reported that 55 million people go below poverty line as a result of funding for their own healthcare.
In sudden death, the patient is likely to suffer minimally, but the family goes through a difficult bereavement. In the other trajectories, the burden of suffering is high and prolonged. It is this “health-related suffering” that palliative care aims to acknowledge, address and help patients and their caregivers adapt to.
What is palliative care?
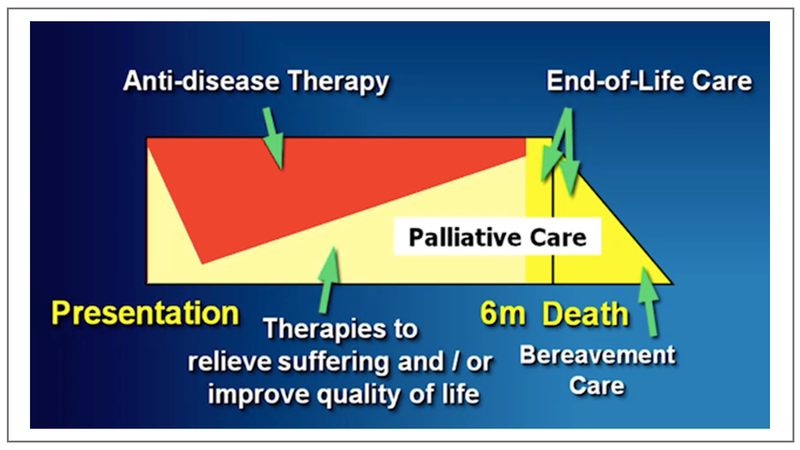
Palliative care by definition is an approach that improves the quality of life of patients and their families facing life-threatening illness, through the prevention and relief of health-related suffering by means of early identification and impeccable assessment and by addressing physical, emotional psychosocial, and spiritual issues. It is a multidisciplinary response to non-preventable deaths that aims at reducing suffering.
Traditionally palliative care has been associated with care of patients with advanced cancer, i.e towards end of life. This is largely the belief even today amongst healthcare professionals and the society.
Statistics show incidence of tuberculosis (39%), pulmonary diseases (6.6%), diarrhoeal diseases in children (6.4%), diabetes + cardio and cerebro-vascular events (4.2%) and malignancy (0.15%) in India.
This clearly shows the escalating trends of non-communicable diseases affecting more Indians and conditions, like diabetes, COPD, ILD, CCF can only be symptomatically controlled through lifestyle changes, exercise, and medications. However, they progress despite optimum treatment.
Doctors are not able to cure all diseases, and must realise that in case of incurable conditions, honest clear communication is vital to prevent breach of trust.
It is this lot of patients that require a holistic approach and integrated palliative care along with curative treatment. In patients with chronic progressive life-threatening conditions it is imperative for health care professionals to sensitively communicate incurablity, prognosis and support that can be provided always to comfort the patients and care for the family.
The journey of a patient with a chronic illness has been compared to falling off the skyscraper in a paper by Fabrizio Elia et al. The way the patient lands depends on how he falls. If his fall is well punctuated by honest, clear discussions about his condition, the family and patient are better prepared to face the eventuality. The patient has time to reflect, think and decide how he should be treated in an emergency. These conversations are difficult, yet when done early, there is time to form a rapport with the patient, improve quality of life by symptomatic treatment and document his wishes regarding care during end of life.
Palliative care is pro-life and at the same time accepts death as a reality especially in non-preventable situations. Research has proved that early-integrated palliative care improves quality and quantity of life in a landmark paper published in 2010. Palliative care can be provided at home, clinic, hospitals and intensive care units not requiring any expensive equipment.**
Life expectancy has increased in India, but this does not translate into better quality of life.
People are living longer, but poorly. Increased life expectancy results in more disease, disabilities, dementia, and pther complications. These bring along burdens of health related suffering to the elderly and their families, especially in countries lacking universal access to palliative care services.
Discussing death and dying is indeed difficult, yet not doing so is worse. It must be pro-actively done in patients with chronic illnesses in order to plan a good death. Conversations cannot be a one off, tick box exercise. There has to be a series of discussions, requiring time to develop trust, and patients should be talking about their personal choices.
When to initiate palliative care?
In the UK, a surprise question has been extensively researched to decide the timing of these conversations. Often, relatives and patients find it unacceptable and inappropriate to have early discussions as it may be demoralising.
The surprise question is, “Will the physician be surprised if the patient is not alive in the next 1 year?” If the answer is no, it is time to start pro-active palliative care.
Gold standard framework suggests indicators for every condition about the timing of pro-active palliative care initiation.
Patients should be approaching end of life if they,
- are likely to die in the next year
- have progressive incurable disease
- are elderly and frail
- have conditions that could cause sudden death
Few will wish to die in an ICU hooked up to monitors and tubes in every orifice, but many of us in India die in this manner. 25% admissions in ICU are not indicated.
- We need to have a paradigm shift in thought processes of physicians, training doctors to communicate effectively to patients about expectations, hopes and fears, not only disease and treatment.
- Palliative care gives doctors and patients a new vocabulary to discuss difficult topics like goals of care in order to have a good death, especially in the context of serious life-threatening illness.
- When a health care institution builds empathy and compassion into the fabric of its operations, it allows clinicians to make time to discuss with a newly diagnosed patient how treatment and illness will affect her, the family, emotions, work, identity and dignity.
- Shared decision making-as against paternalistic should be the way forward. Clinicians must operate in an environment of trust, respect, transparency, and humility. They require the support of the hospital administration to do so.
- Patient autonomy is crucial to decide regarding their medical issues and they must be fully empowered to become equal participants in their own health care.
Coming back to my referral, it was indeed very difficult to talk to the patient and family about the poor long-term prognosis of this young patient. My first task was to find out what they already knew. Based on the information they gave, I clarified details of his medical condition. There was very little curative therapy for him, so it was paramount to palliate his symptoms, focus on quality over quantity of life.
Next was to enquire about his “total pain”. He still had the desire to live, travel and see his children settle. The counselor addressed these issues. The medical social worker intervened as his treatment had left the family in debt. His symptoms worsened despite regular dialysis and diuretics. It was important to explain the futility and poor outcome of aggressive ICU treatment, suggested by his specialists. I sat with the palliative care team and the family to explain this and assured comfort at end of life, to achieve a symptom free dignified end. He died peacefully few hours later surrounded by his wife and son.
As Dame Cicely Saunders, founder of the modern hospice movement quoted:
“The manner in which a loved one passes away is etched in the memories of those who live on”
She believed in this mantra: You matter because You are You. You matter to the last moment of your life. And we will do all we can, not only to let you die peacefully but help you to live until you die.”
Death is inevitable, a bad death is avoidable!
For further reading
- Being Mortal: What really matters in the end. Atul Gawande
- The 2015 Quality of Death Index Ranking palliative care across the world
- New updated GSF Proactive identification guidance (PIG) provides boost for end of life care
(*) (**) Source: Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005;330(7498):1007–1011. doi:10.1136/bmj.330.7498.1007
The author of this article is a Palliative Care Consultant in End-Stage Lung Disease.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries
