Post-COVID neurological symptoms: MoHFW guidelines for management
M3 India Newsdesk Apr 19, 2022
Post COVID-19, there are several acute as well as chronic neurological complications that have been observed. This part of the article series discusses such neurological diseases, their diagnosis and management.
Key takeaways
- SARS-CoV-2, the COVID-19 infectious agent, has a strong affinity for the human angiotensin-converting enzyme 2 (ACE2) receptor.
- Additionally, this receptor is present in neurons and glial cells.
- The prevalence of these symptoms varies between 10% and 87.4% in different studies.
- The extent of investigations required depends on the symptoms or symptom complex, rapidity with which the symptoms progress, severity of these symptoms and the effect of these on the person’s day to day functioning and sense of wellbeing.
- This may be followed for those indulged in extreme physical activities.
- There are no evidence-based specific care guidelines for patients with Post-COVID symptoms.
Findings
Virus particles have been detected in the cerebrospinal fluid and cytoplasm of neocortical and hypothalamic neurons, as well as neuronal degeneration and necrosis, oedema, glial cell hyperplasia, and cellular infiltrates during post-mortem examinations.
It has been proposed that SARS-CoV-2 may stay latent in the central nervous system of healed individuals for an extended period, capable of reactivating and causing neurological problems.
As literature regarding the manifestations of COVID-19 has increased, there has been growing recognition of the long-term sequelae due to this disease. Usually, symptoms are self-limiting and will resolve on their own. It is important to avoid prescribing indiscriminate medication to patients.
Common post-acute COVID–19 neurological symptoms
Numerous investigations have reported inconsistent estimates of post-acute COVID-19 symptoms. According to a recent CDC research, 35% of persons who contracted COVID-19 did not completely recover and continued to have symptoms as follows:
- Fatigue (most common sequelae)
- Changes in concentration
- Impaired memory
- Persistent muscle weakness and myalgias
- Headaches
- Sleep disorders
- Dizziness
- Impairment in smell (Anosmia) and taste (ageusia)
- Rarely new-onset status epilepticus, stroke, acute inflammatory demyelinating\polyneuritis(AIDP), autonomic dysfunction such as orthostatic symptoms
- Non-specific sensory complaints such as paresthesias, numbness, tingling in limbs
Pathophysiology
- Weak immunologic response and incomplete virus eradication resulting in ongoing inflammation
- Genetic predisposition
- Direct invasion of CNS by virus and neurodegeneration
- Dysregulated immune reaction
Risk factors
Probable factors which would predict long term symptoms include:
- Severe COVID-19 requires hospital admission
- Older age
- Obesity
- More than 5 symptoms in the first week of acute COVID-19
Fatigue
- Most commonly reported symptom. The reported frequency is in the range of 16% to 55%.
- It may be assessed using the Chalder fatigue scale. It is an 11-point questionnaire with a Minimum -0, maximum-11 scores and a cut off score ≥ 4.
- If the symptoms are persisting for more than 6 months check whether the condition fits in chronic fatigue syndrome. (the three cardinal symptoms (fatigue, aggravation of symptoms with exercise, and unrefreshing sleep) be present for more than six months and be moderate or severe in severity for at least 50% of the time).
Chronic fatigue syndrome (essential criteria)
- Substantial impairment in the ability to perform activities carried out before the
- Disease for more than six months
- Profound fatigue not relieved by rest
- Discomfort or aggravation after physical exertion
- Unrefreshing sleep
Chronic fatigue syndrome (at least one of the two additional criteria must be present)
- Cognitive impairment (impairment of executive functions or thinking that worsens with exertion, stress or pressure)
- Orthostatic intolerance (symptoms worsen when standing and improve when lying down or raising the lower limbs)
- Patients who meet the criteria for myalgic encephalitis must also have cognitive impairment.
Management of Fatigue
- Self-management and support. No COVID specific guidelines. Look for the other system involvement such as cardiorespiratory and autonomic and refer accordingly.
- Take adequate rest, sleep and maintain hydration. Avoid unnecessarily using over the counter analgesics.
- Management protocol for chronic fatigue syndrome such as graded exercise therapy (GET) may be adopted for selective patients, and self-management strategies such as “pacing” where the patients adjust the activities to avoid exertion may be advised. There are some reports of the utility of Vit-C supplementation.
- Aerobic exercises, balance training, breathing training, and resistance strength training (start with low intensity and gradually raise the duration and intensity) may also be beneficial.
Smell and taste disturbances
Infection with SARS-CoV-2 can lead to chemosensory disorders, with hyposmia/anosmia and ageusia/dysgeusia. These symptoms usually occur during the acute phase and persist. There are no reports of new-onset anosmia or ageusia during the Post-COVID period.
The studies show a median adjusted frequency of:
- Anosmia-23.6% (IQR, 12.4%-40.7%)
- Ageusia or dysgeusia 15.6% (IQR,10.1%-23.9%) during the Post-COVID period
Patients may be asked about the deficit on a Likert scale of 0-10 and the effect on the quality of life may be assessed using
Questionnaire of Olfactory Disorders (QOD) questionnaire. Studies have shown that smell and taste dysfunction recover at a median duration of 31 days. However, some amount of dysfunction may persist in around 1/3rd of people.
Dysautonomia
Dysautonomia can cause:
- Dizziness
- Palpitation
- Exercise intolerance
- Chest tightness
- Presyncope
- And syncope particularly when changing posture from lying to standing
Once the cardiac and respiratory causes are ruled out autonomic dysfunction should be ruled out. One report showed
abnormal autonomic function tests in 12% of patients recovering from COVID-19.
If symptoms are lasting more than 3 months look for the possibility of Postural orthostatic tachycardia syndrome (POTS)
- Increase in HR >30 BPM in adults and 40 in children within 10 minutes of adopting an upright posture
- Absence of postural hypotension
- Symptoms of orthostatic intolerance
- >3 months
Management of Dysautonomia
- Patient education
- Structured aerobic and resistance training and non-orthostatic exercises such as cycling on a recumbent bike/swimming etc.
- Fluid (2-3 L/day) and salt (1-2 tablespoon) supplementation
- Avoid precipitating factors: coffee, alcohol, prolonged standing, hot humid condition and dehydration, drugs such as duloxetine, nortriptyline
- Compression garments
- Pharmacological agents include: Fludrocortisone and midodrine
Headache
- Studies have described varying frequencies of headache during the Post-COVID period ranging from 2-to 60%.
- A recent meta-analysis showed that the frequency of headaches comes down from47% at the time of admission to 8% at 6 months.
- The majority of the patients have tension-type like headache and migraine type headache is less common. However, patients with preexisting migraine can have an increase in frequency.
- Some patients can have features fulfilling daily persistent headache aches.
Management of Headache
- Look for the red flags
- Treatment according to the type and frequency of headache
Cognitive impairment
- Reported in around 12-50% of patients. May persist beyond 1 year. The most frequent deficits are impaired attention, concentration, executive function and memory.
- Brain fog is another common manifestation of Long-COVID, an umbrella term used to describe the constellation of cognitive function impairment such as confusion, short-term memory loss, dizziness, and inability to concentrate. ICU admission and mechanical ventilation during acute illness may contribute to the long-term cognitive impairment.
Management of Cognitive dysfunction
- There is no COVID specific protocol. As in routine clinical practice assess the patient using validated tools and try to rule out treatable causes of cognitive impairment.
- Requires a holistic approach.
- Patients should be assured that most of them will recover.
- Measures such as repeated cognitive exercises, alleviating stress, coping strategies and utilizing the help of speech, language and occupational therapists if available may be useful.
- Engaging in crossword puzzles, simple number games (like sudoku), reading newspapers, and books could help in improving cognitive abilities.
Sleep disorders
- Sleep dysfunction and insomnia can occur in around 18-30%% and may persist beyond one year in the majority.
- The sleep quality may be assessed with the insomnia severity index or Pittsburgh sleep quality index.
Management of sleep dysfunction
- Good sleep hygiene is advised for those having sleep difficulties.
- Avoid caffeine and alcohol use before bedtime, avoid excessive use of phones/computers at bedtime, soothing sleep music in a quiet dimly lit room may help in improving sleep latency.
- Avoid self-medicating with benzodiazepines.
- It is better to consult a doctor than to self-medicate.
Neuromuscular diseases
- Myalgia, fatigue and hyper-CK-anaemia are the most common triad forms (40-70%) of skeletal muscle affection in COVID-19 cohorts.
- Quadriceps and biceps weakness may be found in >75% of survivors of COVID-19 illness and it may persist beyond 1 year even up to 70% of people. – A COVID-19 disease requiring intensive care with invasive ventilation can lead to ICUAW (“ICU- acquired weakness” [ICU: intensive care unit]), a clinical picture in which CIP(“critical illness polyneuropathy”) and CIM (“critical illness myopathy”) intertwine.
- There seems to be no massively increased risk for neuromuscular patients suffering from SARS- CoV-2 infection.
Guillain-Barré syndrome (acute inflammatory demyelinating polyneuritis - AIDP)
- The neurological symptoms usually appear within 5 to 10 days after a COVID-19 diagnosis, although GBS may develop even weeks after infection. Due to the risk of cardiovascular complications, in particular respiratory insufficiency and cardiac arrhythmias, a rapid diagnosis and immediate therapy including critical care admission are recommended.
- Clinically, mild courses up to severe tetraparesis. Cranial nerve involvement with bilateral Facial nerve palsy, ocular muscle palsy or Miller Fisher syndrome is also reported. Often the rapidly progressive course leads to respiratory insufficiency and the need for ventilation.
Management of GBS
- NCS, a demyelinating pattern of damage usually dominates, although axonal processes are also reported.
- CSF diagnosis is necessary to exclude an infectious aetiology. In most cases a cytoalbuminous- dissociation appears. The therapy does not differ from the usual treatment for GBS.
- Intravenous immunoglobulins (2 g/kg BW) are preferred/and plasma exchange also may be considered.
- Corticosteroids should be avoided.
Stroke
Ischaemic strokes and, more rarely, intracerebral haemorrhage (ICH) occur in patients with COVID-19 disease and are associated with a more severe course of the disease. However, strokes have also been reported as Post-COVID sequelae. A confirmed or presumed infection with SARS-CoV-2 in patients with acute stroke should not lead to different treatment than for other stroke patients.
They should receive the same acute diagnostics and acute treatment as all stroke patients, Pathological mechanism involves the following:
- Activation of the coagulation system
- Disseminated intravascular coagulation
- Vascular complications as an expression of severe organ damage
Management of stroke
It is important to recognise stroke symptoms and initiate a Protocol Based Stroke Management. Some of the warning signs are a sudden onset. Some examples include:
- Difficulty in speaking or understanding words
- Loss of feeling or strange feeling on one side of the body
- Weakness of the face, arm or leg on one side of the body
- Unexplained dizziness or loss of balance
- Decreased or blurred vision
- Severe unexplained headache
Since the window for thrombolysis is 4.5 hours a quick assessment should be made fast. Following are some pointers:
- Ask the patient to smile
- Ask the patient to raise their arms
- Ask the patient to say a phrase
- And ask about the time of onset of symptoms
Refer the patient to a centre with a stroke management facility if needed
Epilepsy
Patients with chronic epilepsy have reduced access to doctors and drugs and can therefore suffer drug withdrawal attacks. For this reason, it is important to ensure that patients with pre-existing epilepsy always have access to outpatient neurological care and sufficient and timely antiepileptic drugs are prescribed to prevent supply shortages. As part of Post-COVID syndrome status epilepticus has been reported.
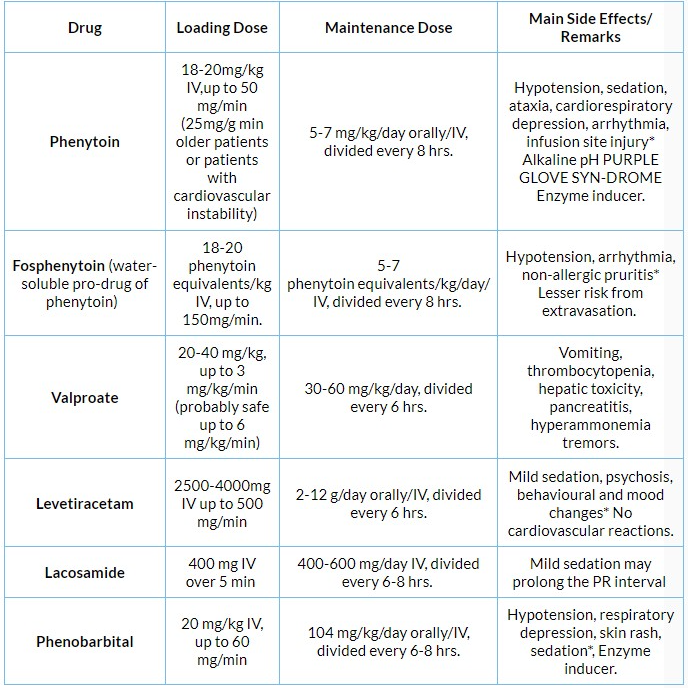
Management of Status Epilepticus:
Management plan does not differ in Post-COVID conditions compared to routine management. When the aetiology is unclear and CSF does not suggest infection a more detailed investigation may be useful, including Anti-N-methyl-D- aspartate (NMDA) antibody and Anti-voltage gated potassium channel antibody. Investigations such as CSF, brain imaging, EEG and drug monitoring etc. are to be used judiciously.
- First Line agents- Lorazepam/Diazepam/Midazolam
- Second-line agents- Phenytoin/fosphenytoin/sodium valproate/ Lacosamide/Levetiracetam/Phenobarbitone
- Refractory SE- Irrespective of the timeframe, SE that persists despite adequate administration of benzodiazepines and at least one antiepileptic drug is labelled refractory SE (RSE).
- More aggressive measures should be taken, with intubation and mechanical ventilation of the patient and frequently hemodynamic support with pressors or inotropes.
- Drugs such as propofol, Thiopentone, ketamine and midazolam may have to be used Patients may be referred to higher centres in case of unresponsiveness.
Diagnosis and management of Post-COVID sequelae
History
Take a precise history of the onset of the first COVID-19 symptoms. Enquire regarding persistent fatigue decreased ability to exercise, decreased ability to carry out routine daily activities, slowness in thinking, attention, concentration, confusion (Post-COVID fog), dizziness, persistent headachesand sleep issues (increased sleep latency and/or maintenance).
Examination:
- Vitals (Blood pressure, pulse rate and rhythm, respiratory rate, pulse oximetry and saturation among all COVID-19 survivors).
- Cognitive assessment: Mini-mental status examination / Montreal Cognitive Assessment Test. / 6-IT test as a screening tool among those having cognitive complaints. Detailed lobar function testing in those having an abnormal MMSE.
- Detailed neurological examination (including power testing) in those complaining of muscle aches, myalgias, and persistent weakness in limbs.
- Sensory examination to rule out objective sensory loss among those presenting with sensory symptoms of paresthesias, pin-pricking, tingling and numbness.
Investigations for Post-COVID patients with neurological sequelae:
The extent of investigations required depends on the symptoms or symptom complexity, rapidity with which the symptoms progress, the severity of these symptoms and the effect of these on the person’s day to day functioning and sense of wellbeing.
- Hemogram with ESR
- Liver function tests
- Kidney function tests
- Fasting blood sugar
Specific investigation among COVID-19 patients with neurological sequelae/symptoms:
- CPK (those with muscle aches, myalgias and persistent weakness).
- Nerve conduction studies for Patients having sensory-motor complaints about suspected neuropathy including Guillain Barre syndrome after a thorough neurological examination.
- CSF analysis: Only to be considered for select patients with severe cognitive, persistent neuropsychiatric or behavioural issues (to rule out other causes, active meningoencephalitis or Post-COVID autoimmune-mediated encephalitis) or suspected immune-mediated neuropathy is suspected.
- Patients with brain fog or cognitive neurological dysfunction should be administered a higher cognitive function assessment.
- Brain MRI may be required in selected patients with worsening and significant cognitive neuropsychiatric manifestations.
- Patients suspected to have autoimmune involvement in the nervous system should undergo a detailed assessment for autoimmune antibodies.
- Autonomic function studies: Start with measuring blood pressure and heart rate after 5 minutes of lying supine, and then 3 minutes after standing. Orthostatic hypotension may be diagnosed if there is a fall of >20 mmHg systolic and >10 mmHg diastolic after standing for 3 minutes. For detailed evaluation in indicated cases, tertiary care referral may be required.
- EEG - For patients with status epilepticus if a non-convulsive status is suspected.
- Polysomnogram- In patients with significant sleep dysfunction for which tertiary care referral may be done.
- Patients with mild innocuous symptoms may be thoroughly examined and followed up at appropriate intervals. The patients may present with multisystem symptoms.
Care and follow-up of Post-COVID patients:
- Depending on the presentation of an individual the patient appropriate generally accepted guidelines for management and care of patients should be followed. There are no evidence-based specific care guidelines for patients with Post-COVID symptoms.
- The duration of some of the symptoms or sequelae of some of the Post-COVID illnesses is not as yet clearly defined. Usually, symptoms are self-limiting and will resolve on their own.
- It is important to avoid prescribing indiscriminate medication to patients. Formal consultations are sparingly used only for selected patients with severe persistent symptoms.
Therapeutic options under trial
- Nicotinamide riboside, a dietary supplement, for cognitive symptoms and fatigue.
- Use of monoclonal antibodies such as Leronlimab and tocilizumab for the management of Post-COVID syndrome
When to return to work
- There is a consensus expert recommendation that besides 2 weeks of convalescence, one should have a normal electrocardiogram and transthoracic echocardiography before returning to competitive sports and this may be followed by those indulged in extreme physical activities.
- The first 2 weeks of exercise should be minimal exertion, with gradual progression with self-
Monitoring of symptoms.
IV Antiepileptics for management of SE
The guidelines for post COVID sequel by MoHFW will be discussed in this series pertaining to different organ systems- Cardiovascular, Gastrointestinal, Nephrological, Neurological, and Respiratory. Click here to read the previous parts- Post-COVID cardiovascular sequelae: Latest MoHFW updates, Gastrointestinal symptoms post COVID-19: New MoHFW updates, Post-COVID nephrology related conditions: MoHFW guideline updates.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries