Neurological Emergencies: Rapid Diagnosis and Management Strategies
M3 India Newsdesk May 01, 2024
Neurologic emergencies demand swift diagnosis and treatment to prevent severe outcomes like long-term disability or death. This article offers in-depth insights into acute stroke, subarachnoid haemorrhage, status epilepticus, and other critical conditions, catering to non-neurologist physicians.
Acute ischaemic stroke: Time is of the essence
About 85% of strokes are ischaemic, resulting from diminished vascular supply to the brain.
Symptoms such as:
- Facial droop
- Unilateral weakness or numbness
- Aphasia
- Gaze deviation
- Unsteadiness of gait may be seen
Time is of the essence, as all currently available interventions are safe and effective only within defined time windows.
Diagnosis and assessment
- The National Institutes of Health (NIH) stroke scale is an objective marker for assessing stroke severity as well as evolution of disease and should be obtained in all stroke patients.
- Scores range from 0 (best) to 42 (worst).
- Laboratory assessments should encompass a fingerstick blood glucose test, coagulation analyses, a full blood count, and a fundamental metabolic panel.
- Patients with ischaemic stroke who present within 4.5 hrs hours of symptom onset should be considered for intravenous administration of tissue plasminogen activator (tPA), a safe and effective therapy with nearly 2 decades of evidence to support its use.
Acute haemorrhagic stroke: Blood pressure, coagulation
Approximately 15% of strokes are caused by intracerebral haemorrhage, which can be detected with non-contrast head CT with a sensitivity of 98.6% within 6 hours of the onset of bleeding.
Chronic inadequately managed hypertension is a frequent root cause of intracerebral haemorrhage, leading to the rupture of weakened vessels, termed "lipohyalinised," resulting in blood leakage into the brain tissue.
Treatment of acute haemorrhagic stroke
- Early aggressive therapy, targeting a systolic blood pressure goal of less than 140 mm Hg within the first hour, is safe and can lead to better functional outcomes than a more conservative blood-pressure-lowering target.
- Short-acting antihypertensive agents in intravenous form, such as nicardipine and labetalol, are frequently used.
- Reversal of any coagulation abnormalities should be done quickly in intracranial haemorrhage.
- There is a growing trend towards utilising alternative agents, such as prothrombin complex concentrate (available in both three- and four-factor preparations) and recombinant factor VIIa, to swiftly reverse anticoagulation, in addition to traditional options like vitamin K or fresh-frozen plasma.
Subarachnoid haemorrhage
The sudden onset of a “thunderclap” headache (often described by patients as “the worst headache of my life”) suggests subarachnoid haemorrhage.
Unlike intracranial haemorrhage, where blood accumulates within the brain, subarachnoid haemorrhage primarily occurs in the spaces containing cerebrospinal fluid surrounding the brain. This condition often results in an increased risk of hydrocephalus due to compromised drainage of cerebrospinal fluid.
Diagnosis and management of subarachnoid haemorrhage
- Non-contrast CT of the head is the main modality for diagnosing subarachnoid haemorrhage.
- Blood within the subarachnoid space is demonstrable in 92% of cases if CT is performed within the first 24 hours of haemorrhage, with an initial sensitivity of about 95% within the first 6 hours of onset followed by CT angiography can safely exclude aneurysmal subarachnoid haemorrhage and obviate the need for lumbar puncture.
- Early management of blood pressure for a ruptured intracranial aneurysm and Aneurysms are treated (or “secured”) either by surgical clipping or by endovascular coiling.
- Endovascular coiling is the preferred option when it can be safely performed alongside other treatment modalities.
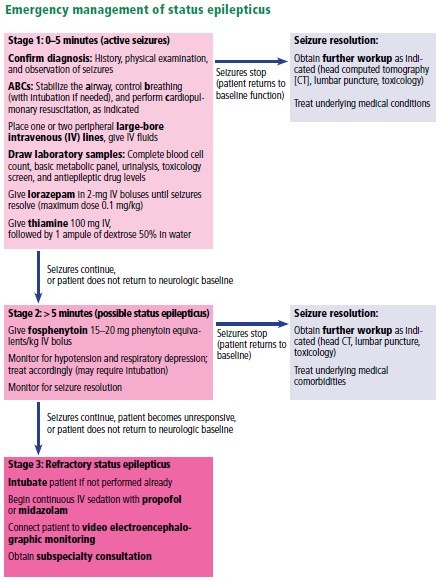
Status epilepticus: Seizure control is important
Any seizure lasting longer than 5 minutes continuously or recurring without the patient regaining consciousness between episodes should be managed as status epilepticus. All types of seizures pose the risk of evolving into status epilepticus, and the effectiveness of antiepileptic medications decreases as seizure duration increases.
Once the ABCs of emergency stabilisation have been performed (i.e., airway, breathing, circulation), antiepileptic drug therapy should start immediately using established algorithms.
Throughout treatment, the accuracy of neurological assessments might be compromised by medication side effects or persistent status epilepticus, necessitating frequent use of continuous video electroencephalographic monitoring to direct subsequent therapy for patients who are slow to improve. Head CT scans with contrast or magnetic resonance imaging are valuable for identifying any structural anomalies that could underlie seizures.
Routine laboratory tests, including toxicology screening, can detect common triggers like hypoglycemia or stimulant ingestion. Further investigation is warranted for signs of meningitis, such as fever, through cerebrospinal fluid analysis.
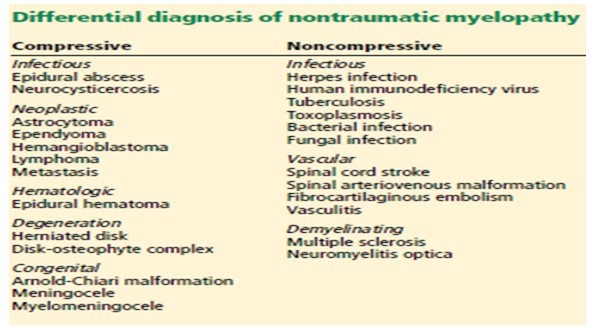
Spinal cord injury: Traumatic myelopathy
Acute spinal cord injury can lead to substantial long-term neurologic impairment and should be suspected in any patient presenting with focal motor loss, sensory loss, or both with sparing of the cranial nerves and mental status. Causes of injury include compression (traumatic or non-traumatic) and inflammatory and noninflammatory myelopathies.
Basic management of spinal cord injury includes decompression of the bladder and initial protection against further injury with a stabilising collar or brace. Magnetic resonance imaging with and without contrast is the ideal study to evaluate injuries to the spinal cord itself. Although CT scans are useful for detecting spinal column fractures, they are not effective in visualising internal spinal cord abnormalities.
The guidelines recommend maintaining mean arterial pressure above 85 to 90 mm Hg during the initial 7 days following traumatic spinal cord injury, especially challenging in cases of hemodynamic instability associated with lesions above the mid-thoracic level.
Methylprednisolone therapy for acute spinal cord trauma remains contentious, with meta-analyses showing inconclusive benefits.
Neuromuscular disease: Is ventilation needed?
Diseases involving the motor components of the peripheral nervous system share the common risk of causing ventilatory failure due to weakness of the diaphragm, intercostal muscles, and upper-airway muscles. Clinicians need to be aware of this risk and view these disorders as neurologic emergencies.
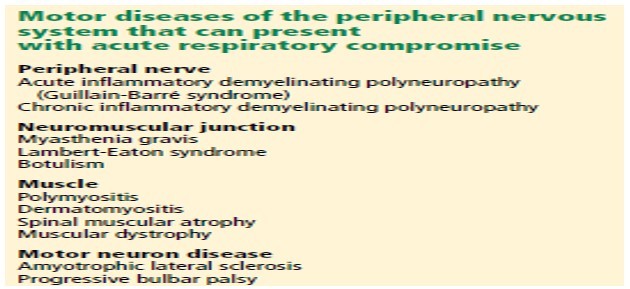
Myasthenic crisis
Myasthenia gravis results from autoantibodies targeting postsynaptic acetylcholine receptors, leading to muscle weakness, typically in a proximal distribution.
Symptoms include:
- Fatigue
- Respiratory difficulties
- Nasal speech
- Ophthalmoparesis
- Difficulty swallowing
Exacerbations can occur as a response to recent infection, surgery, or medications such as neuromuscular blocking agents or aminoglycoside.
Myasthenic crisis, while uncommon, is a life-threatening emergency characterised by bulbar or respiratory failure secondary to muscle weakness. Intubation and mechanical ventilation are frequently required.
Patients with myasthenia gravis who experience delayed extubation beyond 24 hours postoperatively should be regarded as being in crisis.
Diagnosis: The diagnosis of myasthenia gravis can be confirmed through serum autoantibody testing, electromyography, and nerve conduction studies, including repetitive stimulation. Alternatively, edrophonium administration can be employed in patients displaying evident ptosis.
The mainstay of therapy for myasthenic crisis is either intravenous immunoglobulin at a dose of 2 g/kg over 2 to 5 days or plasmapheresis (5–7 exchanges over 7–14 days).
Treatment: Corticosteroids are not recommended in myasthenic crises in patients who are not intubated, as they can potentiate an initial worsening of the crisis. Once the patient begins to show clinical improvement, outpatient pyridostigmine and immunosuppressive medications can be resumed at a low dose and titrated as tolerated.
Acute inflammatory demyelinating polyneuropathy (Guillain-Barré syndrome)
Acute inflammatory demyelinating polyneuropathy is an autoimmune condition characterised by the presence of autoantibodies targeting axons or myelin in the peripheral nervous system.
This disorder should be suspected in patients experiencing worsening muscle weakness, typically accompanied by areflexia, over a period of days to weeks.
Occasionally, recent systemic infections like diarrhoea may serve as triggers. Autonomic nerve involvement can manifest as blood pressure fluctuations and cardiac arrhythmias. While traditionally described as "ascending paralysis," other variants such as descending paralysis and Miller-Fisher syndrome may present with distinct clinical features like ataxia, areflexia, and ophthalmoparesis.
Diagnosis is typically confirmed through electromyography, nerve conduction studies, and cerebrospinal fluid analysis, which often reveals elevated protein levels and few white blood cells.
Treatment involves intravenous immunoglobulin or plasmapheresis, as corticosteroids have shown limited effectiveness. Given the progressive nature of the disease, anticipating ventilatory failure and preparing for intubation is crucial.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Nikhil Repaka is a Neuro physician at Jagruth Super Specialty Hospital, Khammam.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries